Printable Soap Note Template
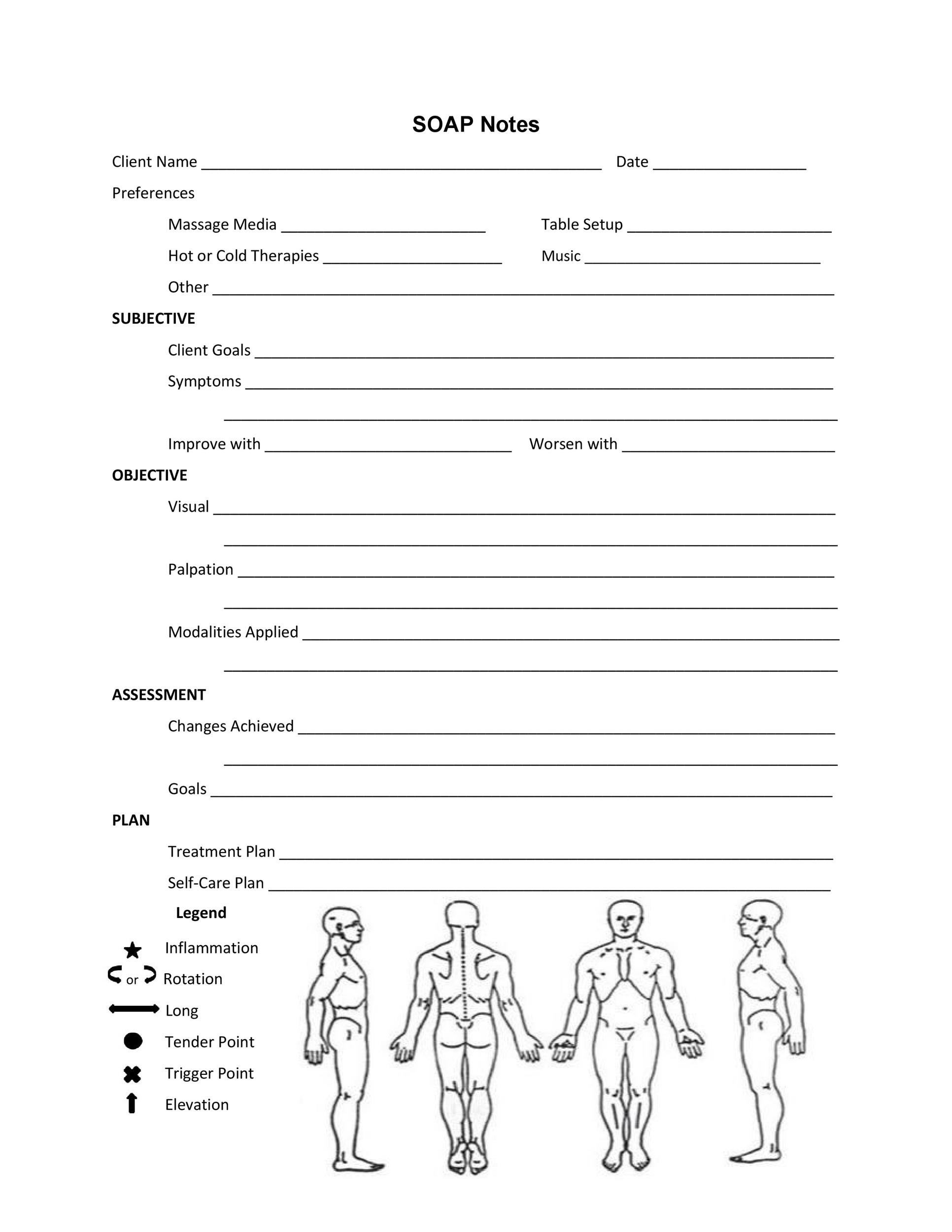
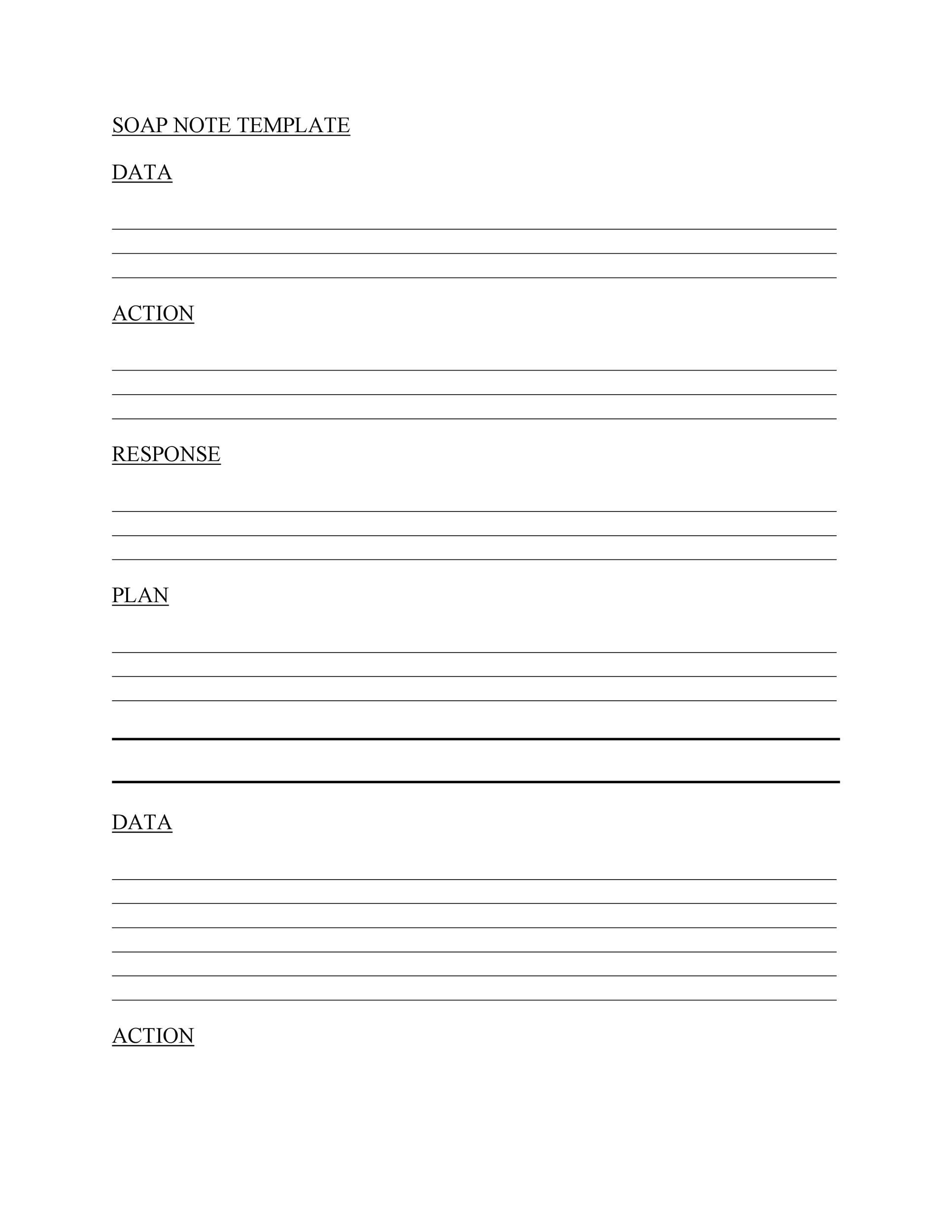
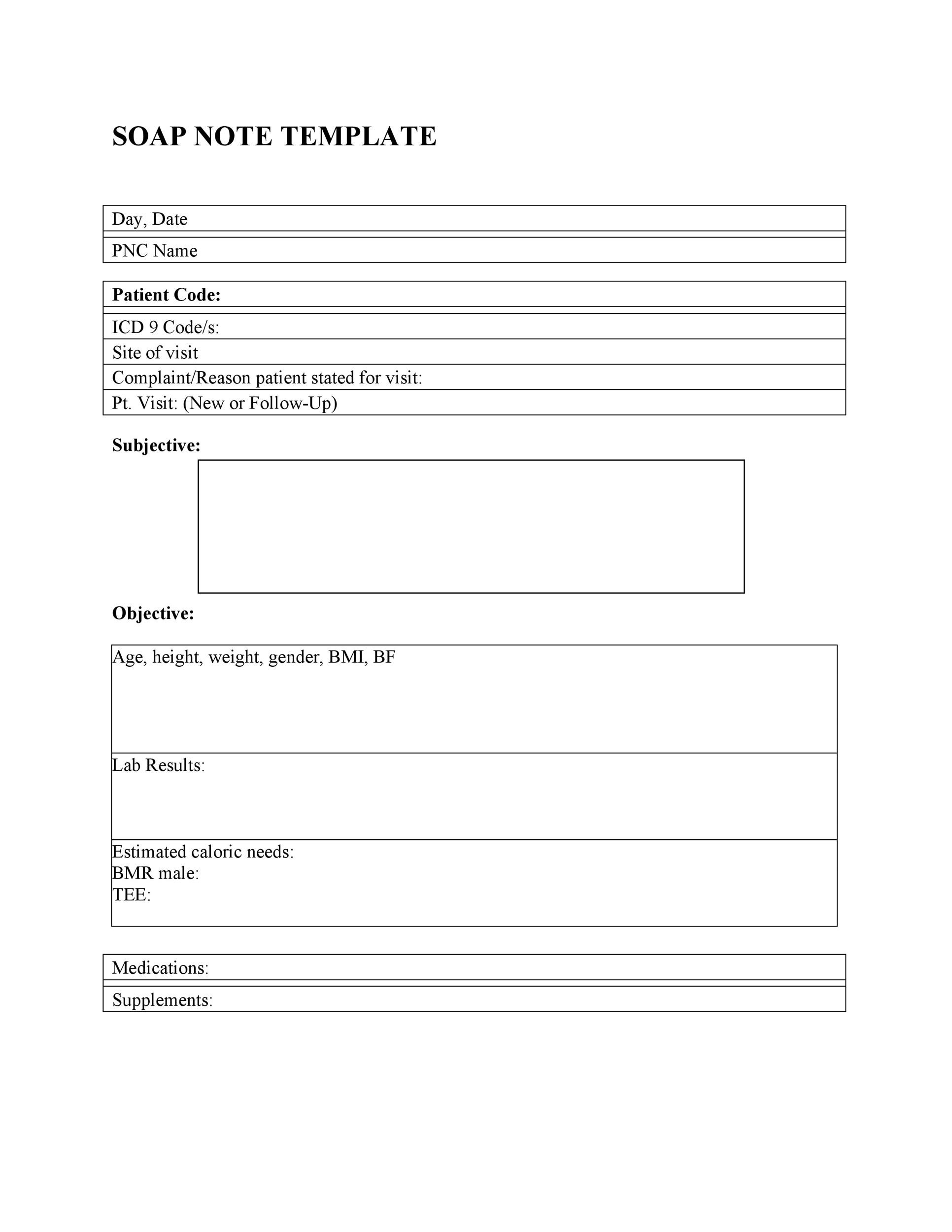
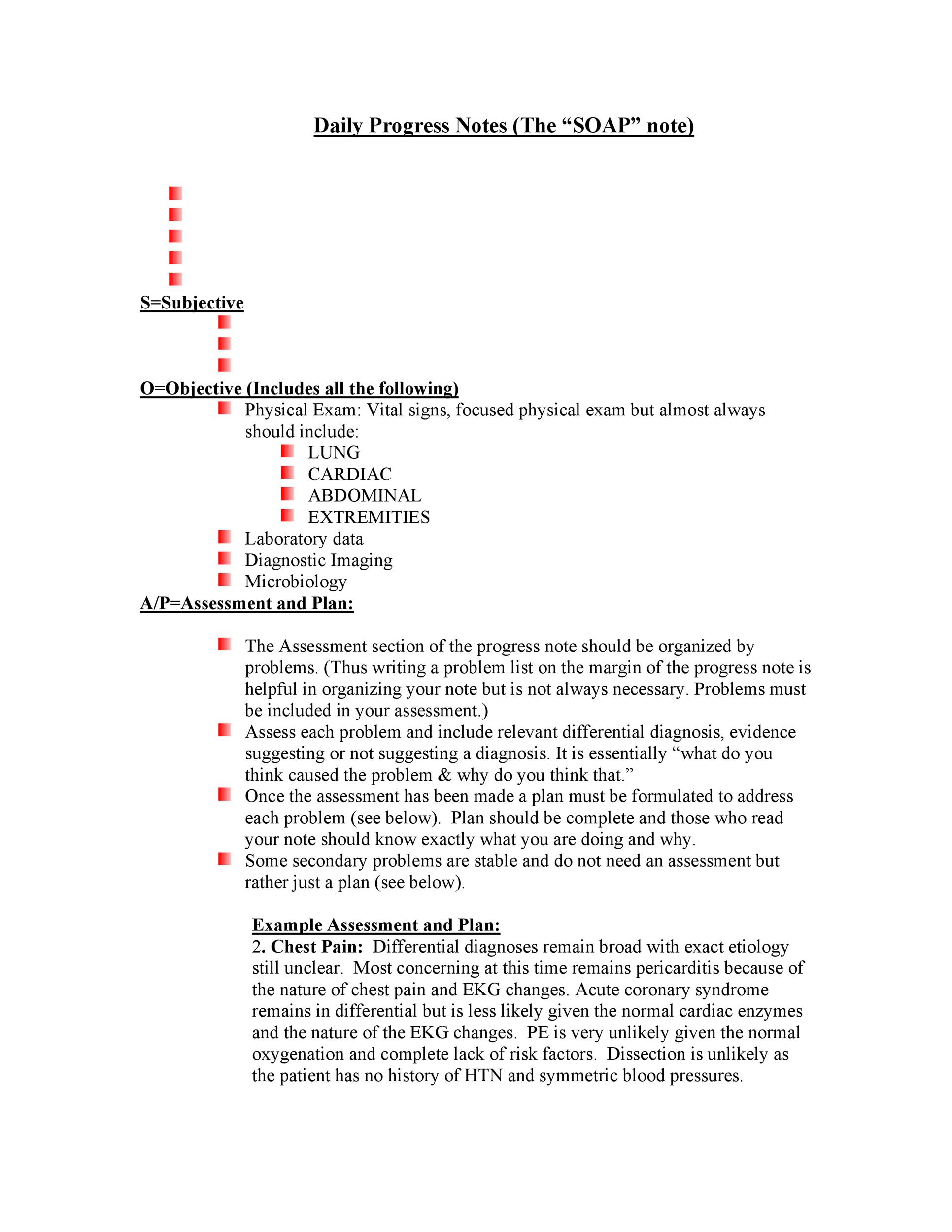
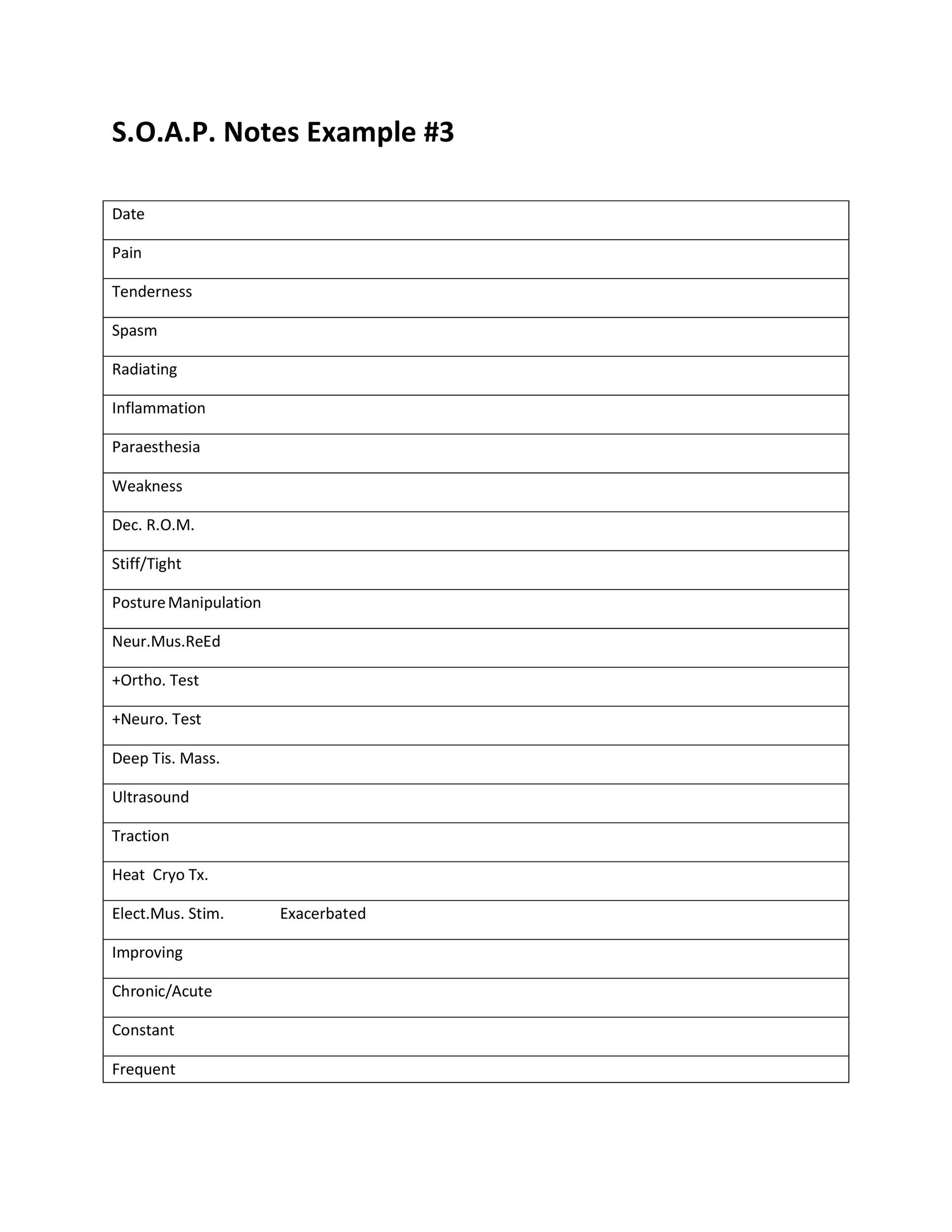
Printable Soap Note Template - So what are soap notes? Web download our comprehensive soap note pdf template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes: Physical therapy soap note template. Download template download example pdf. Web what is a soap progress note template? Web 40 fantastic soap note examples & templates. Soap notes are a helpful method of documentation designed to assist medical and mental health professionals in streamlining their clinical notes. Soap notes in mental health practice. Web free soap notes form. Web this template has the four sections of soap notes laid out for you already, with space for you to fill them in as you interact with your patient, as well as space for you to fill in your patient’s details. Soap notes are another words for a specific type of patient documentation form, for which soap is an acronym used to remember the four sections of the form: Web soap note templates. Web download our soap notes template pdf file right now. Soap notes are written documentation made during the course of treatment of a. Modernize and streamline patient assessments. Soap stands for subjective, objective, assessment, and plan, which are the key components of a soap note. Web download our soap notes template pdf file right now. Web soap note template 01. One of the best parts about using clinical soap notes is how easy it is to follow. Try it out for free. Web printable & editable soap note examples & templates in word, pdf & excel. Health professionals must have an accurate record of their patients. So what are soap notes? Soap notes are another words for a specific type of patient documentation form, for which soap is an acronym used to remember the four sections of the form: Find free downloadable. Web learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. Soap stands for subjective, objective, assessment, and plan, which are the key components of a soap note. Health professionals must have an accurate record of their patients. Try it out for free. Soap notes are a notetaking format used broadly within the. Web free soap notes template. The soap acronym stands for the four sections of the note: Subjective, objective, assessment and plan. Using a template such as soap notes means that you can capture, store, and interpret your client's information consistently over time. Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not. Web printable & editable soap note examples & templates in word, pdf & excel. Eliminate paperwork with digital checklists. Find free downloadable examples you can use with clients. 2 what do you write in a soap note? How to use this soap note template pdf? Mental health providers will find soap notes beneficial for creating treatment plan documentation in particular. Although soap notes were initially developed for use in medical settings, they have become increasingly popular in mental health practice due to their clear and concise format. Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not. Physical therapy soap note template. Try it out for free. Web soap note templates are standardized forms used by healthcare professionals, such as doctors, nurses, and therapists, to document patient encounters and medical assessments in a structured and organized manner. Find free downloadable examples you can use with clients. Although soap notes were initially developed for use in medical settings,. Web this template has the four sections of soap notes laid out for you already, with space for you to fill them in as you interact with your patient, as well as space for you to fill in your patient’s details. With a solid grasp of the soap acronym, you as a practitioner can improve the informative power of your. Subjective, objective, assessment and plan. Web learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. Web soap note templates. Web 3 helpful templates and formats. Although soap notes were initially developed for use in medical settings, they have become increasingly popular in mental health practice due to their clear and concise format. Web get the free printable soap note template. Soap notes are written documentation made during the course of treatment of a. Modernize and streamline patient assessments using paperless soap note templates and a soap note example for nursing. Find free downloadable examples you can use with clients. Web 40 fantastic soap note examples & templates. Soap notes are a helpful method of documentation designed to assist medical and mental health professionals in streamlining their clinical notes. S ubjective (summary), o bjective (observations), a ssessment, and p lan. Include symptom dimensions, chronological narrative of patient’s complains, information obtained from other sources (always identify source if not the patient). Web download our comprehensive soap note pdf template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes: Web this template has the four sections of soap notes laid out for you already, with space for you to fill them in as you interact with your patient, as well as space for you to fill in your patient’s details. Soap stands for subjective, objective, assessment, and plan, which are the key components of a soap note. Web learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. Free to use for up to 10 users. Soap (subjective, objective, assessment and plan) notes are used at intake and ongoing to document a client's condition and progress. If not, let’s learn all about it. Check out these free soap templates to elevate your clinical documentation, and improve accuracy, productivity, and clinical outcomes.
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab
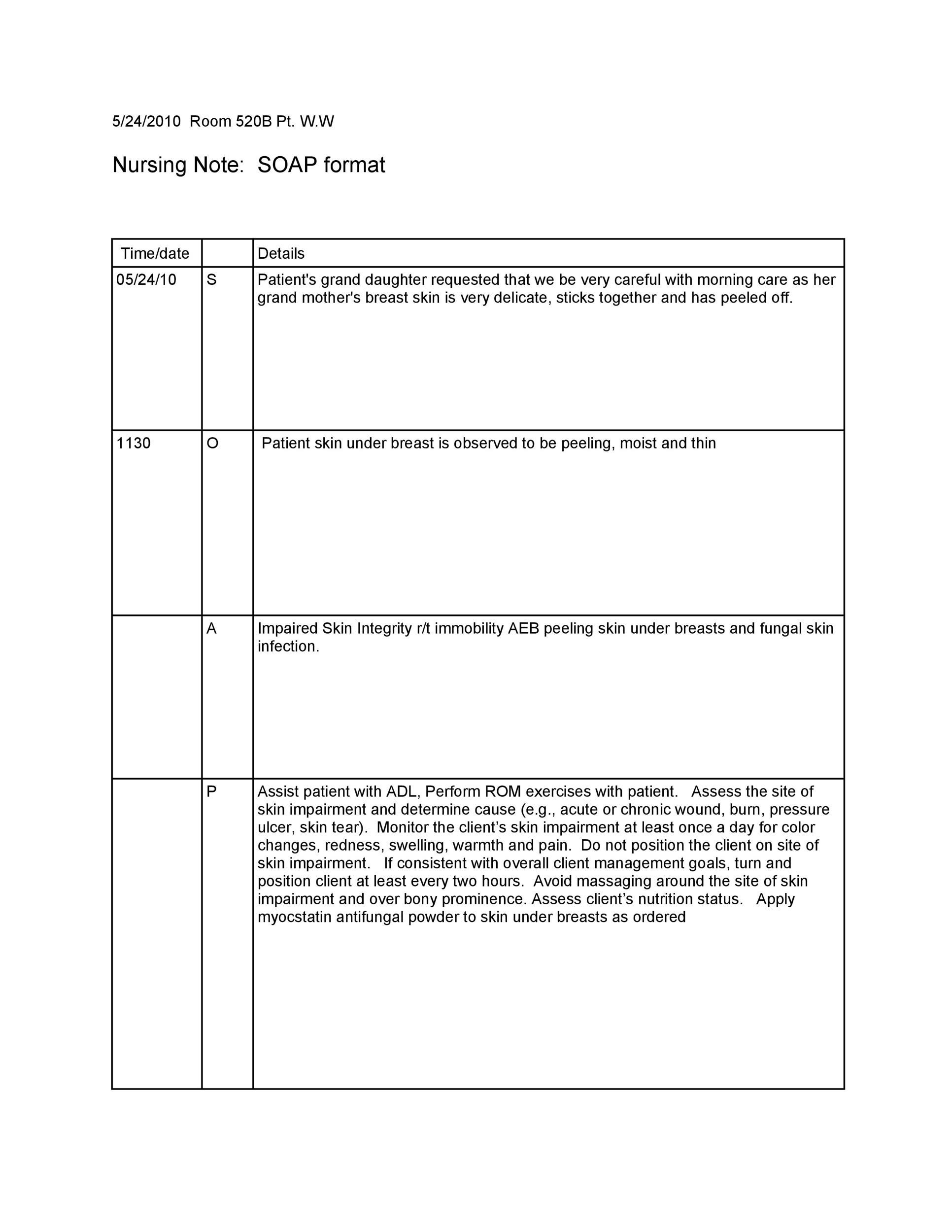
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab

Printable Soap Note Template tomtaku

Soap Note Fillable Form Printable Forms Free Online
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab

10+ Soap Note Template Free Download Word, Excel, PDF Format!!
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab
40 Fantastic SOAP Note Examples & Templates Template Lab
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab
The Templates Are Available In Pdf Format And The File Size Starts From 15Kb.
Mental Health Providers Will Find Soap Notes Beneficial For Creating Treatment Plan Documentation In Particular.
If You Have Worked Or Are Currently Working In A Hospital, You Probably Already Know What A Soap Note Is.
One Of The Best Parts About Using Clinical Soap Notes Is How Easy It Is To Follow.
Related Post: